Serration Technology for the Treatment of Arteriovenous Fistulas
Introduction
Maintaining the patency of arteriovenous (AV) fistulas remains a significant challenge in patients requiring hemodialysis. Despite being the preferred form of vascular access, AV fistulas are prone to complications following intervention, particularly elastic recoil, inadequate luminal gain, and restenosis. These mechanical and biological challenges contribute to poor long-term outcomes and frequent reinterventions.
Challenges
Elastic recoil is a major factor limiting the success of percutaneous transluminal angioplasty (PTA). Following balloon deflation, vessel walls often elastically return toward their pre-procedural state, leading to significant residual stenosis and early failure. Recent studies have reported primary patency rates after angioplasty as low as 44% at 12 months, reflecting the persistent impact of recoil and neointimal hyperplasia (NIH)1. Inadequate luminal gain compounds this problem. Lesions in AV fistulas are often highly fibrotic or calcified, making them resistant to full expansion, even with high-pressure non-compliant balloons. Under-expanded lesions not only compromise immediate blood flow but also contribute to rapid restenosis.
Restenosis remains one of the most prevalent causes of AV access failure. Mechanical injury from PTA accelerates NIH. Longer lesion length, the presence of multiple stenoses, and high shear forces have all been associated with higher recurrence rates1. Despite high technical success rates immediately after intervention, durability remains poor, with freedom from reintervention often falling below 50% within the first year.
To address these challenges, stenting is sometimes used in AV fistula interventions. However, the role of stents is generally reserved for salvage cases. While stents are beneficial in preventing early collapse or recoil, they do not address the underlying processes of restenosis and NIH. Stenting is not a universal solution, and in many cases, it may only delay the need for further interventions. It may also introduce long-term complications, including infection, thrombosis, difficulty in accessing the fistula for future procedures and loss of opportunities for further proximal AV accesses.
These realities underscore the growing importance of vessel preparation and more effective primary therapies in AV fistula management. Traditional high-pressure and scoring balloons can help, but there remains a significant unmet need for technologies that both optimize luminal gain and minimize vessel trauma to reduce recoil and restenosis. Moreover, successful vessel preparation is crucial not only to create a larger, more sustainable lumen but also to establish a favorable vessel environment when pharmacologic therapies, such as drug-coated balloons (DCBs), are used.
Recent randomized controlled trial data have demonstrated that DCB angioplasty can improve 12-month patency rates compared to plain-old balloon angioplasty (POBA), but these benefits depend heavily on adequate vessel preparation2.
Solution
In this context, the Serranator® PTA Serration Balloon Catheter represents a novel approach to addressing the dual challenges of vessel preparation and primary therapy for AV fistula interventions.
The Serranator uses stainless steel micro-serration technology, designed to create linear, interrupted scoring along the endoluminal surface. With 1,000x more point force compared with POBA, serration occurs during slow-and-low balloon inflation and is designed to aid vessel expansion, effectively optimizing luminal gain in all lesion morphologies with minimal recoil.
The Serranator offers a compelling solution for treating AV fistula stenoses—particularly in challenging lesions where traditional POBA may be insufficient. The Serranator has proven to be effective in treating peripheral artery disease and chronic limb-threatening ischemia, and its unique mechanism of action holds promise for addressing similar challenges in AV fistula management, providing a potential solution to improve outcomes and reduce the need for repeat interventions. Several case studies follow which illustrate the utility of Serranator angioplasty use for AV access-related complications.
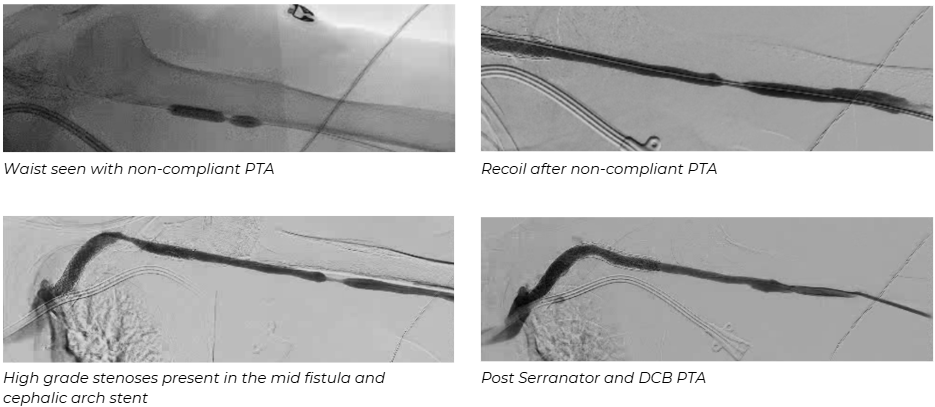
Case 1: Serranator use for recoil after non-compliant balloon PTA and in-stent restenosis
Presentation
A late 60-year-old female with a left brachial-cephalic AV fistula created 5 years prior, presents with prolonged bleeding and poor dialysis clearance. A duplex demonstrates stenosis in the proximal segment and in-stent restenosis in the cephalic arch stent.
Procedure
Antegrade access was obtained in the distal fistula and a 6 Fr sheath was inserted. A fistulagram was performed demonstrating >90% stenosis in the mid fistula as well as >85% in-stent restenosis in the cephalic arch stent. PTA of both lesions was performed with a non-compliant 6 x 40 mm balloon but significant recoil was encountered with >50% residual stenosis. PTA was then performed with 6 x 40 mm Serranator balloon followed by a 7 x 60 mm DCB angioplasty. Completion angiography demonstrated <30% residual stenosis with a strong thrill present. The patient’s symptoms resolved and the patient had >1000 mL/min volume flow on follow-up duplex. She has not required repeat fistulagram at last follow-up 12 months post-procedure.
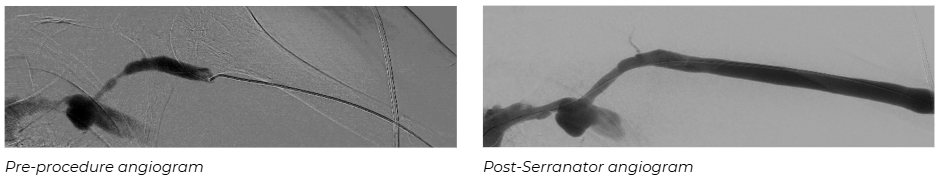
Case 2: Brachial artery PTA in a patient with steal syndrome and hostile anatomy
Presentation
A mid 70-year-old female with prior left arm AV graft infection, who underwent graft explantation 12 weeks ago by another surgeon, now presents with severe hand pain and ulceration of her index finger. Arterial duplex suggests brachial artery stenosis proximal to the fistula. Due to the anticipated significant scar tissue burden from her graft explantation, an upper extremity angiogram with intervention was recommended.
Procedure
Femoral arterial access was obtained and a 5 Fr sheath was inserted. The left subclavian and axillary arteries were cannulated with use of a 0.035” wire and angled catheter. A left upper extremity arteriogram was performed demonstrating critical stenosis of the brachial artery proximal to the AV anastomosis. The sheath was exchanged for a 6 Fr sheath advanced into the subclavian artery. Multiple attempts were made to cross the lesion in an antegrade fashion but were unsuccessful. Therefore, the left radial artery in a retrograde fashion was accessed and via a micropuncture sheath, a 0.014” wire was used to cross the lesion. The wire was snared and the brachial artery was angioplastied with a 2.5 x 40 mm Serranator followed by a 5 x 40 mm Serranator balloon. This was followed with 5 x 40 mm DCB angioplasty. Completion angiography demonstrates <10% residual stenosis with intact distal run off to the hand and palmar arch. The patient had a palpable radial pulse, multiphasic ulnar artery signal on completion. Her finger ulcer healed within 2mos following the procedure and her brachial artery remains patent without significant residual stenosis 14mos post-procedure.

Case 3: Avoidance of stent placement
Presentation
A late 60-year-old male with a left brachial-cephalic arteriovenous fistula, which has become progressively aneurysmal, presents with high grade stenoses seen in the venous outflow on duplex imaging. He had undergone 3 prior fistulagrams with POBA of the venous outflow at a referring center in 2-3 month intervals but continues to suffer from severe arm edema and prolonged bleeding.
Procedure
Antegrade access was obtained in the distal fistula and a 6 Fr sheath was inserted. A fistulagram was performed demonstrating >90% stenosis of the cephalic venous arch. The lesion was crossed with a 0.018” wire. PTA was performed with a 6 x 40 mm Serranator balloon followed by 7 x 60 mm DCB angioplasty. Completion angiography demonstrated <30% residual stenosis and the patient had a strong thrill. The patient did not require repeat fistulagram or stent placement for over 9 months at follow-up before he passed away from a myocardial infarction.
Conclusion
AV fistula dysfunction remains a major barrier to reliable dialysis access, with restenosis, elastic recoil, and poor luminal gain limiting the durability of percutaneous interventions and leading to frequent reinterventions in a population already facing significant lifestyle disruptions. The cases presented highlight the challenges of complex and variable lesion morphology, and the limitations of standard PTA.
The Serranator® PTA Serration Balloon Catheter proved effective across a range of difficult scenarios—resolving recoil, treating in-stent restenosis, addressing inflow disease in hostile anatomy, and avoiding stent placement. Its use led to improved vessel expansion, reduced recoil, and extended patency, with patients experiencing prolonged symptom-free intervals. Unlike conventional PTA, the Serranator's serration technology offers precise vessel modification while minimizing trauma. When combined with DCB angioplasty, it may enhance drug uptake and further reduce NIH.
These early results suggest the Serranator is a promising alternative to traditional PTA for AV fistula stenosis, particularly in challenging cases. Its ability to optimize vessel preparation and reduce procedural complications supports its role in a more durable, intervention-sparing treatment strategy for dialysis access maintenance. Notably, these cases demonstrated excellent outcomes using the 5.0 and 6.0 mm diameter Serranator devices. With larger sizes on the horizon, the technology’s utility is poised to expand even further across a broader range of AV access interventions.
References
1) Zheng Y, et al. Predictors associated with early and late restenosis of arteriovenous fistulas and grafts after percutaneous transluminal angioplasty. Ann Transl Med. 2021;9(3):242. PMID: 33569434 2
2) Li X, et al. Drug-Coated Balloon Angioplasty for Dysfunctional Arteriovenous Hemodialysis Fistulae: A Randomized Controlled Trial. Clin J Am Soc Nephrol. 2023;18(1):34-42. PMID: 38191561