Successful Serranator After Failed POBA in a Critical Limb Ischemia Patient
PATIENT PRESENTATION
A woman in her early 70s was referred to our clinic after a previous lower extremity arteriogram was obtained for a non-healing right foot ulceration 3 months prior. After her intervention, the patient experienced persistent rest pain and no wound healing. Her focused exam was significant for nonhealing ulcers on her right foot/digits and no palpable pedal pulses.
DIAGNOSTIC ASSESSMENT
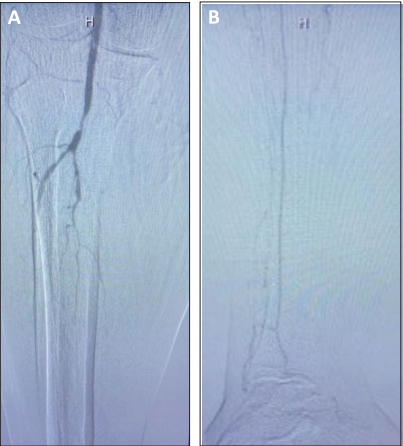
Arterial access was performed in the contralateral limb. Initial angiography revealed high-grade stenosis of the P3 segment of the popliteal artery and severe tibial disease (Figures A and B). The prior arteriogram revealed significant tibial disease, including a 50-cm CTO in the distal tibial artery that was left untreated. It did not show any baseline popliteal lesions; however, following the balloon angioplasty, there was a small dissection plane that remained untreated that likely caused this new popliteal lesion.
INTERVENTION
Given the anatomy and location of the wounds, revascularization of the popliteal and AT artery was the interventional goal to provide in-line, angiosome-directed flow to the foot, facilitate wound healing, and prevent amputation. Using a 0.014-inch Glidewire Advantage guidewire and a 0.018-
inch NaviCross support catheter, the CTO was crossed down to the DP artery. Orbital atherectomy with the Diamondback 360 (Cardiovascular Systems, Inc.) was performed with a 1.25-mm
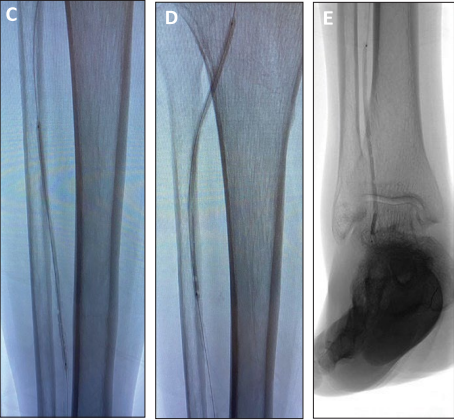
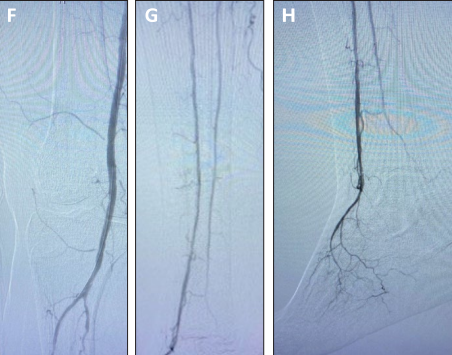
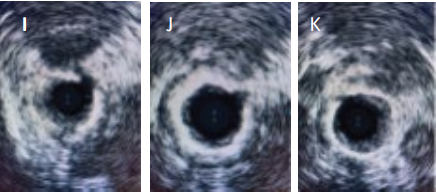
Micro Crown. Following channel creation, serration of the lesion was performed with sequential Serranator balloons at low atmospheres through the full lesion (Figure 5A-5C). Final angiography showed significant luminal gain, no recoil, and brisk flow (Figure 6). Intravascular ultrasound (IVUS) was also performed after the intervention, which demonstrated an open tibial artery with visible serrations into the medial layer of calcification (Figure 7). A Tack endovascular system (Philips)
was placed in the previous popliteal dissection.
CONCLUSIONS
Pulsatile blood flow was restored to the foot, and the patient was referred to a wound clinic for ongoing management. After 8 weeks, her rest pain had resolved and a minor amputation procedure was planned.
Any thoughts looking back on this case?
Dr. Siah: It’s important to point out these lesions are increasingly common, and we need a better solution than what has been done before. As we saw in this case, POBA was not an effective treatment to restore blood flow to the foot. Additionally, the luminal gain provided by effectively sized serration resulted in markedly improved perfusion to the foot compared to her previous intervention.
Why did you choose to use the Serranator PTA balloon in this case?
Dr. Siah: For a couple of reasons, in my previous experience with the Serranator device, I have seen impressive luminal gain after serration, without dissections or any significant recoil. Secondly, the patient already failed POBA, so I know I needed an alternative technology if we were going to try to prevent amputation. The size of this patient’s vessels and her underlying comorbidities made her a challenging candidate for bypass, as well as her absence of autogenous conduit. Sequential Serranator balloon catheters were used to serrate the full length of the lesion. Serranator 2.5 X 120 mm at 3 atm (C), Serranator 3 X 120 mm at 3 atm (D), and Serranator 2.5 X 120 mm at 3 atm (E).
Final angiography showed significant luminal gain, no recoil, and brisk flow after Serranator use
(F - H). IVUS images showing open tibial artery with visible serrations into the medial layer of
calcification (I – K) I J K
In this case, you utilized atherectomy in combination with the Serranator PTA balloon. How do you see these two modalities working together?
Dr. Siah: Tibial CTOs can be very challenging to treat. I am a firm believer that atherectomy, particularly orbital atherectomy, can facilitate delivery of therapy in heavily diseased, small blood vessels. Not only does it allow for effective device delivery, but it allows for full luminal expansion at lower angioplasty pressures. That goes hand in hand with the effectiveness of the Serranator device— which aims to deliver point force along the entirety of the target treatment area at low balloon pressures, which in turn likely leads to more predictable, durable outcomes
without the development of dissections.
How has the availability of the Serranator PTA balloon changed your practice when treating BTK lesions?
Dr. Siah: It has given me a new tool to treat complex patients. When I am treating a BTK lesion, whether it’s a focal stenosis or a long-segment CTO, I think about utilizing the technology. Its low-pressure, focal force mechanism has repeatedly demonstrated predictable results that have been impressive; I’ve seen fewer dissections on IVUS, and as a result, my cases have become less complicated. They’ve become shorter—I do not need to re-balloon areas due to dissection or recoil or pull other devices off the shelf to treat flow-limiting
dissections.
How do you anticipate this device changing your treatment algorithm in above-the-knee lesions?
Dr. Siah: Its application above the knee is very exciting. I think, in conjunction with drug-eluting technology, we could have a game-changer in our hands. We will be able to deliver drug to parts of the artery that haven’t been able to be reached before this point, and as someone who tries not to leave any metal behind during an intervention, I am optimistic that we will see “stent-like” results angiographically and hopefully into longer-term follow-up. What that ultimately means is increased durability of our interventions, leading to less repeat interventions for patients and, ultimately, fewer amputations for our patients and decreased cost to our health care system.